Dentists will likely be feeling the pain too during your next visit.
After losing over a month’s worth of revenue following guidelines from the Centers for Disease Control and Prevention to provide only emergency services, dentists are eager to see their patients again.
But doing so comes at a hefty cost.
To lure patients back and ensure his own safety as well as his staff’s, Anthony Ceccacci, a dentist and owner of Madison Avenue Smiles, a New York City-based dental practice, said he’s gone on a financial limb with scant guidance from health authorities.
For $85, he’s offering finger-stick antibody tests. He’s also asking all of his patients to rinse their mouths with iodine prior to being seen.
“ ‘At this time, the ADA does not have a formal policy on antigen testing.’ ”
He’s spent nearly $35,000 on disinfectant equipment such as oral high-speed aerosol evacuation units, ozone generators and ultraviolet lights.
After donating masks and other forms of personal protective equipment (PPE) to frontline health-care workers in New York City, he’s now being priced out of N95 masks, surgical gowns, face shields and goggles which dentists are now required to wear per CDC guidelines.
On Tuesday, Republican Sen. Susan Collins from Maine voiced concerns from dentists in her state who have been unable to see patients, which she said “is causing growing health problems.” She asked Robert Redfield, head of the CDC, whether existing guidelines were adequate enough for dentists to return to work.
“We’ve been interacting and talking with dentists, and working with the state and local public-health physicians to update our guidelines on reopening a variety of medical services,” Redfield said during a Senate COVID-19 hearing held Tuesday. “We are in the process of updating those guidelines and they will include direct guidelines for dental practices.”
Aside from PPE and a one-page coronavirus screening questionnaire for patients, Ceccacci said, “It’s been crickets” from the New York State Dental Association as well as the American Dental Association. “The guidance from them has been so poor. They’ve given me no clear directive.”
“If I were to bring back my staff following their recommendation, how can I look them in the face and say they’ll be safe?” Ceccacci said.
“ ‘If I were to bring back my staff following their recommendation, how can I look them in the face and say they’ll be safe?’ ”
In a toolkit for interim reopening guidelines the ADA published in early May, there is no mention of the disinfecting equipment he bought or antibody testing.
“At this time, the ADA does not have a formal policy on antigen testing,” said Matthew Messina, a Columbus, Ohio-based dentist who serves as a spokesperson for the ADA.
“Dentists who I have spoken to are very appreciative of the guidance of the ADA, and their state and local dental associations during this pandemic,” he added.
That’s certainly not the case for Ceccacci, who has instead taken cues from Kwang-Bum Park, a well-known South Korean dentist who runs a multi-practice clinic based in the Daegu metropolitan area, the country’s coronavirus epicenter.
“South Korea has gone through it already,” Ceccacci said, which is why he looks to Park over the ADA. The ADA and the NYSDA, he added, are “all about protecting themselves.” He said they’re treading cautiously to avoid being criticized later. “I don’t blame them, but I didn’t expect any direct answers from them on how to reopen my office.”

In a tool kit for interim reopening guidelines the ADA published in early May, there is no mention of the disinfecting equipment he bought or antibody testing.
Anthony Ceccacci
The ADA and other dental associations rely on advice from the CDC
Last week, Chad Gehani, president of the ADA penned a letter to the CDC asking the agency to “quickly provide guidance on how to safely reopen dental practices during the deceleration phase of the COVID-19 outbreak.”
“The latest CDC guidance (of April 27) is still appropriate for those parts of the country where COVID-19 infection rates are accelerating or peaking,” the letter stated. “However, the situation is much different in areas where infection rates are now declining — and the risk(s) of acquiring or transmitting COVID-19 are very low. It is critical for dentists to have a new or revised guideline recognizing a risk-based approach.”
“ Chad Gehani, president of the ADA penned a letter to the CDC asking the agency to ‘quickly provide guidance on how to safely reopen dental practices during the deceleration phase of the COVID-19 outbreak.’ ”
“The CDC appreciates the letter from the American Dental Association and is actively adjusting its response and guidance as conditions change and as we learn more about COVID-19,” said Kate Fowlie, a spokeswoman for the CDC.
“The CDC has been working recently on updating the COVID-19 guidance for dental settings in preparation for resuming care. We anticipate the updated guidance will be available soon.”
Although dentists in 31 states are allowed to reopen and perform elective procedures, the CDC recommends dentists only provide emergency services. As it stands, the agency does not have any published protocol on how to safely offer non-emergency services.
But for emergency care, the CDC says, “If a surgical mask and a full face shield are not available, do not perform any emergency dental care. Refer the patient to a clinician who has the appropriate PPE.”
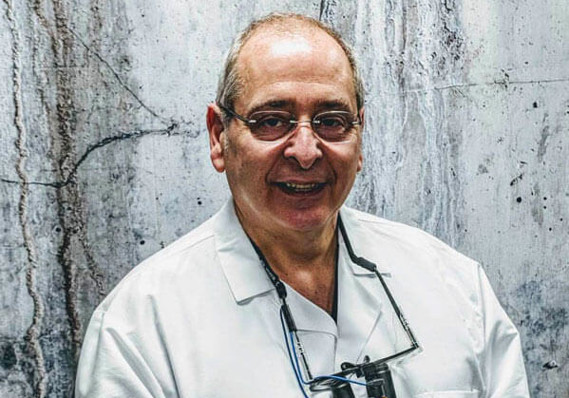
Anthony Ceccacci, a dentist and owner of Madison Avenue Smiles, a New York City-based dental practice.
Anthony Ceccacci
Reputations are on the line
During the AIDs crisis, Ceccacci said dentists had “a bad runup” and were seen by some people as a mechanism for transmitting the deadly disease.
Recalling a story published in The New York Times in 1993 regarding a Florida dentist who allegedly had unintentionally caused six of his patients to contract AIDS, Ceccacci said, “I don’t want to be that guy.”
“ During the AIDs crisis, dentists were seen by some people as a mechanism for transmitting the deadly disease, helped by a 1993 story in The New York Times. ”
To avoid that, he’s gone above and beyond in terms of preparing his office to see patients next month, assuming that New York Gov. Andrew Cuomo, a Democrat, doesn’t issue new guidance that would push back the date.
“I’ve always considered every patient as a potential for disease, but coronavirus has taken it to the next level,” Ceccacci added. “We’ve just enhanced our office’s protocol because of the patient’s fear and anxiety. If they don’t see us donned in hazmat suits, they’ll think they’re not safe.”
“I have invested a lifetime in this multimillion-dollar practice, if I lost it have no idea what my next career would be.”
Similarly, Jeremy Peyser, a dentist based in New York City, recognizes that one allegation of a patient contacting COVID-19 from visiting him could be fatal for his practice.
That’s why he stopped seeing patients in early March when one of his employees called in sick. She said she had a fever, and Peyser encouraged her to get a coronavirus test, but at the time, such tests were not available unless you were in an at-risk category or had recently visited a COVID-19 hot spot.
Since then, he has only been seeing patients who need emergency care. But he won’t just see any patient. “It has to be someone I know and have seen personally,” he said. “If I don’t really know them how would I know if they’re practicing social distancing?”
Unlike Ceccacci, Peyser has held off on purchasing new disinfecting equipment until the ADA or CDC share “what works and what doesn’t work” in terms of killing coronavirus, he said.
“ Jeremy Peyser, a New York City-based dentist, says that one allegation of a patient contacting COVID-19 from visiting him could be fatal for his practice. ”
In the meantime he’s been relying on a Whatsapp FB, +1.96% group composed of New York City-based periodontists, oral surgeons and general dentists like himself.
Members of the group share new information, especially concerning protocol for reopening their offices, disinfecting equipment and the CARES Act’s Paycheck Protection Program.
Like the 12 other people in the chat, Peyser was not able to obtain a PPP loan in the first round. In the second round he was approved for a $44,000 loan which made it possible for him to bring back staff he had to furlough. This comes at a time where the number of Americans working in dental offices has plunged by more than 53% since February, according to the Bureau of Labor Statistics.
The group chat has also been a forum for industry experts to share their own insights on how to safely reopen and discuss new equipment. They take care to distinguish between opinion and facts when sharing information. He adds, “My opinion can only be so helpful.”
Before coronavirus, Michael Scialabba, rarely worried about having enough gloves and masks for all 260 clinicians across 76 different dental practices he oversees as vice president of clinical affairs for 42 North Dental, a New England-based dental-service organization.
He simply placed an order with the same wholesale supplier. Occasionally, shipments would come in late or get lost in the shuffle. But when more patients were admitted to hospitals due to coronavirus in mid-March, his supplier told him that they couldn’t sell anything to him and that everything “was going to hospitals.”
“ ‘When you have to buy from multiple suppliers and you don’t have a relationship with them you’re low on the totem pole.’ ”
At that time, all 76 locations had enough surgical masks to get by, but then the CDC recommended dentists wear N95 masks even for patients that don’t display coronavirus symptoms.
Suppliers placed limits on how many masks one customer could buy, which was far less than “what you would need in order to see patients,” Scialabba said.
Instead of having just one supplier, he’s buying from over six. There’s also no guarantee that the masks and other PPE will make it to his office, Scialabba added. He also worries that delivery drivers will end up keeping the masks for themselves.
If that happens, he said it would be nearly impossible to get refunded. Compounding the problem: He’s paying more for gowns, face shields, gloves and masks than before.
“When you have to buy from multiple suppliers and you don’t have a relationship with them you’re low on the totem pole,” Scialabba said. “It’s really the Wild West out there.”
Prior to the pandemic he said an N95 mask cost $1.50. And now? He’s paying $12 per mask. What’s more, gowns that “used to cost pennies” are now going for $4 to $6.
“ ‘Dental practices need to return to full essential service, not just emergency services, for the health of the public.’ ”
“Most of our offices haven’t been open for eight weeks, so we’ve had no capital inflow,” Scialabba added. Despite that, he’s paying $8,000 to $10,000 more on PPE per office.
Peyser and Ceccacci are facing the same problem.
In addition, Peyser said that the suppliers he’s in touch with “can’t even guarantee me a price because they don’t know how much they’re going to have to pay for inputs on their end.”
Both donated PPE to frontline health care workers in New York City and are now being priced out of PPE.
“Dental practices need to return to full essential service, not just emergency services, for the health of the public,” said Mark Feldman, executive director of the NYSDA.
But when it comes to obtaining affordable PPE, the organization said it has “no comment at this time.”
To afford these premiums, Scialabba has advocated for a new insurance code to bill for infection-control fees, which the ADA signed off on.
Now he’s able to charge some patients an additional $10 per visit given that not all insurance companies are on board. While this hardly covers the full cost of PPE especially when a patient needs to see multiple providers, “it helps mitigate the cost and show that we’re all in this together.”
Ultimately, Scialabba is worried about patients who stop going to the dentist altogether.
“That’s the last thing I want to see,” he said. “This could easily cause an oral health crisis if everyone stops seeing their dentists.”