MADRID — Just days away from the start of a new school year, Spain’s capital city rolled out fresh restrictions on Monday to cope with what’s becoming a relentless second wave of cases.
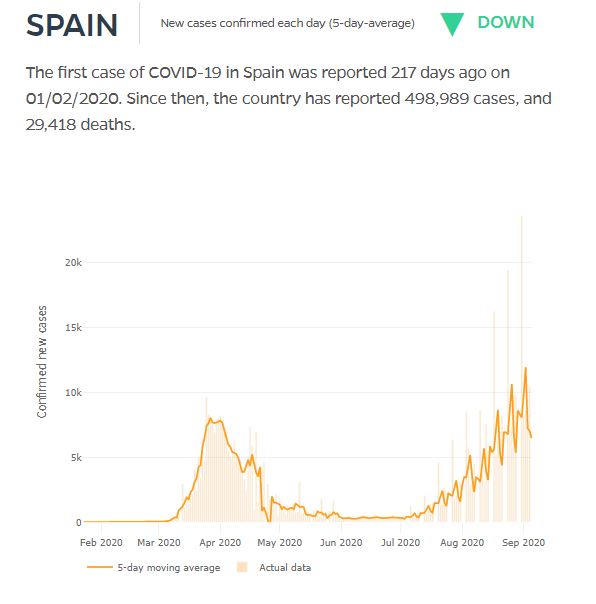
But those measures — strict controls on the distance between seats rather than tables in food-service settings, reducing funeral attendance to 25 people indoors and 50 outdoors, and 10-person limits on social gatherings — seem modest as the country’s total infections close in on 500,000, according to the latest data from Johns Hopkins. Official numbers indicate that threshold has already been reached. Spain’s is the highest infection total in Europe, though it pales against the 6 million–plus cases in the U.S., which has seven times Spain’s population.
Madrid’s new measures are cold comfort to parents, including this journalist, who will be sending at least one child to all-in-person classes of 21 children. More than 2,000 of 66,000 Madrid teachers recently tested positive for COVID-19 and will have to be retested. Elsewhere in the country, two schools have already had to close due to infections.
At the heart of the resurgence of Spain’s cases has been a rush to return to normal. Spain’s experience has also been impacted by government desperation to get the tourism industry and bars back in operation; overly relaxed family gatherings; insufficient safety protocols for field workers; and the behavior of idle youth with effectively nothing to do but party, and spread the virus.
Much as New York did, Spain climbed out of the depths of COVID-19 infections with the strictest measures possible, but Spain fell right back two months later. How the country pulls itself out this time may be a blueprint for other countries and municipalities to follow. MarketWatch spoke to these experts via email in hope of shedding light on where Spain stands now and what should be done.
Juan Jesús Gestal Otero, professor emeritus of preventative medicine and public health at the University of Santiago de Compostela in Galicia, was one of 20 experts who signed a letter in the British medical journal the Lancet asking for an independent review of Spain’s COVID-19 response.
MarketWatch: What key mistakes did Spain make after the lockdown in the spring, and what must it do now to fix the situation?
Otero: It took a long time to get contact tracing up and running. It should have started when the case curve began to decline. It would have helped to have the disease more controlled at the end of the de-escalation. Each autonomous community set up its own tracking system, many of them insufficiently staffed.
MarketWatch: Will Madrid’s new measures, such as cutting capacity at bars and restaurants, really help get the disease under control?
Otero: I don’t think those measures help much to contain outbreaks. … To have the disease under control, the most important thing at this time is to strengthen the tracking capacity of the national health system. If this is not done soon, the continued increase in outbreaks can eventually overwhelm the tracking capacity of the system and lead to a loss of control and aggravate the situation. National coordination is also very important.
Don’t miss:To defeat COVID-19, ‘we need a unified national strategy,’ says public health expert Dr. Howard Koh
MarketWatch: What are the differences between now and March that are encouraging and discouraging?
Otero: Now there is epidemiological surveillance capacity, although it needs much improvement, for the early diagnosis of cases and contact tracing, and there is the capacity to perform many tests, which allows for detection of a large number of asymptomatic patients. Most of the current cases are young people in whom the disease is less severe, unlike in March-April, and the health system is not under pressure. It is discouraging to observe how certain social groups, mostly young people, are encouraging outbreaks with their behaviors.
MarketWatch: What should other countries learn from Spain?
Otero: Strongly strengthen the epidemiological surveillance system. As soon as possible, start tracking the contacts of the cases and carry out many, many tests, to locate the largest possible number of asymptomatic patients. Make the return to the “new normal” very carefully to avoid new outbreaks. Do not authorize activities that are incompatible with a respiratory pandemic, such as those that involve spending time in closed, poorly ventilated places with many people, parties, nightlife activities. … Raising awareness of the need to take protective measures in homes when they receive visitors, receive them in well-covered rooms, avoid family parties … as it is in homes where the greatest number of infections occurs.
Dr. Vicente Soriano is the director of the UNIR Medical Center in Madrid and a clinician and professor of infectious diseases at the UNIR Health Sciences School and Medical Center.
MarketWatch: What do you think of Madrid’s new measures to try to contain the virus?
Soriano: The confluence of crowding, the return to working activities for many, and easier access to testing — as compared with negligible in March — largely accounts for the new surge in cases. It will go up for the next couple of weeks. Despite, to date, that many new PCR+ diagnoses have been found in young and asymptomatic people, this second wave will soon expand to the whole population, including again the most vulnerable populations. Indeed, although so far the situation at most large Madrid hospitals has not collapsed, it reminds us slightly of what happened in February, when overwhelming began to occur.
MarketWatch: What about contact tracing and other efforts?
Soriano: The advent of rapid antigen tests will be helpful, although there is room for further improvement, testing saliva (instead of nasopharynx fluid), selling in pharmacies, and allowing for self-testing at home, like pregnancy tests, as many times as convenient.
MarketWatch: What else needs to be done?
Soriano: Regional governments need to work further on three areas: (1.) increase the role of primary-care physicians as a first barrier to assess nonseriously ill patients and manage them with the help of telemedicine, avoiding the collapse of hospital emergency departments; (2.) medicalization and ensure enough health-care workers and protective equipment for nursing homes for the elderly and other institutionalized patients — these places accounted for more than 60% of the death toll during the first COVID-19 tsunami wave in Spain; (3.) ensure stocks of diagnostic tests, protective equipment and enough doctors and nurses in clinics and hospitals for confronting the new COVID-19 surge. Acting upfront is always preferable to at the time of demand, when damage has already occurred.
MarketWatch: As a parent, how do you feel about sending your own children back to school?
Soriano: Reopening schools is a critical decision that is supported by the fact that youngsters very rarely become sick and allows parents to continue their jobs. So, I am in favor of reopening schools and therefore let my four children go to school, with the maximum guarantees they have established. I am aware that temporal closing of groups, classes and periodic cases will be reported. Inevitable. But working under this threat is preferable to paralyzing or closing the school.
Read on:Top coronavirus doctor in Spain has a message for revelers and tourists









