MarketWatch photo illustration/iStockphoto
MarketWatch photo illustration/iStockphoto Coronavirus. It’s just like the flu, isn’t it?
Hundreds of thousands of people die of the flu every year, some say, and people need to calm down about coronavirus, which was declared a pandemic by the World Health Organization Wednesday.
Everyone should wash their hands for 20 seconds, elbow bump, stop buying face masks because they don’t protect against the virus, note that airplane air is filtered 20 to 30 times an hour, avoid cruise ships, and just relax.
That appears to be the accumulated advice of exasperated Americans on Twitter and Facebook FB, -4.46% who despair at the long lines at Trader Joe’s and Whole Foods AMZN, -3.75% (where people apparently have been stocking up on oat milk), and the panic buying and empty shelves at Costco COST, -3.87%. “Toilet paper is golden in an apocalypse,” one customer told MYNorthwest.com. They’re overreacting, right? Not quite.
‘This is additive, not in place of. Yes, the flu kills thousands of people every year, but we’re going to have more deaths.’
On Monday, President Trump wrote on Twitter TWTR, -8.77%, “Last year 37,000 Americans died” from the flu: “Nothing is shut down, life & the economy go on,” he added. On Wednesday, the president announced that he was “marshaling the full power of the federal government” by suspending all travel from Europe to the U.S. for one month.
As this dramatic change-of-heart illustrates, we still have a lot to learn about the novel coronavirus and, experts say, that alone should be enough to motivate communities to work together to slow its progress. Studies suggest the differences between the flu and coronavirus are more nuanced than some people suggest.
In fact, health professionals point out important distinctions between COVID-19, the disease caused by coronavirus SARS-CoV-2, and other viruses. They don’t advise mass hysteria, obviously, but nor do they believe doing nothing and/or going about your business as usual is a smart move either.
On Wednesday, WHO said coronavirus has become a pandemic. WHO had characterized the illness late last year as a series of epidemics. An epidemic is a disease that infects regions or a community., such as the 1918-19 “Spanish flu” or, one of the most extreme pandemics ever recorded, the Black Death from 1347 to 1351.
So what are the differences between coronavirus and the flu? For starters, there is no vaccine for COVID-19 and it could take many months or years to get one to market, and, unlike the influenza viruses for which there are several vaccines, humans have not built up an immunity over multiple generations. What’s worse, doctors fear the virus will mutate.
The first known person was reported to have contracted the virus on Dec. 1 in China. Today, it’s spread to nearly 100 countries. Experts advise changing your behavior to limit its spread. Public officials in New York have said people should avoid taking mass transit, if possible. Italy has effectively quarantined its entire population. Israel has closed its land borders.
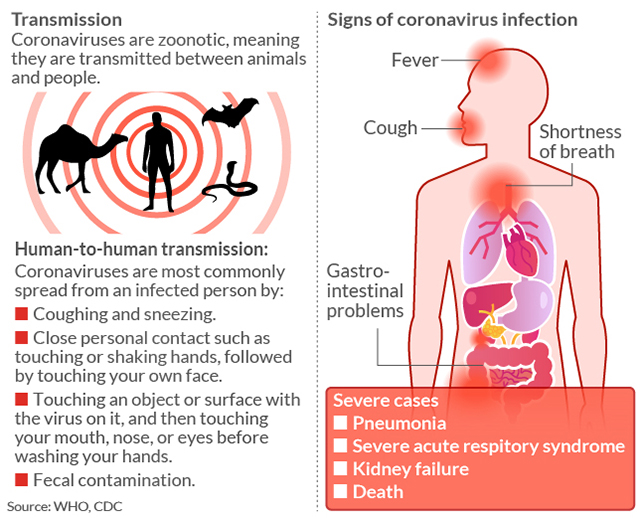
Of course, there are similarities between influenza and COVID-19. Both viruses are untreatable with antibiotics, and they have almost identical symptoms — fever, coughing, night sweats, aching bones, tiredness and, in more severe cases of both viruses, nausea and even diarrhea. They can be spread by touching your face, coughing and sneezing.
But doctors say their differences are just as varied. “It’s a little simple to think the novel coronavirus is just like flu,” Amesh Adalja, a senior scholar at the John Hopkins Center for Health Security and a spokesman for the Infectious Diseases Society of America, told MarketWatch.
“We don’t want another flu,” he said. “This is additive, not in place of. Yes, the flu kills thousands of people every year, but we’re going to have more deaths.”
There are reported to be some 1 billion influenza infections worldwide each year, with up to 45 million cases in the U.S. per year, tens of thousands of U.S. deaths, and 291,000 to 646,000 deaths worldwide.
Seasonal flu has a fatality rate of less than 1%. Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases on Capitol Hill, estimates that the fatality rate of flu is closer to 0.1%. But even accounting for the mild, yet undiagnosed cases of COVID-19, he said Wednesday, it would still make it “roughly 10 times more lethal than the seasonal flu.”
Another reason not to compare the two viruses: Influenza has likely been around for more than 2,000 years. Scientists say the “novel influenza A viruses” in humans lead to a pandemic approximately once every 40 years. But, again, flu vaccines exist. “The flu has been with us since the birth of modern medicine,” said Adalja.
Flu has likely been around for 2,000 years. This coronavirus is three months old and, as yet, there is no vaccine.
Hippocrates of Kos, the Greek physician who was born around 460 BC, mentioned what we now know as the modern influenza virus in his writings, some historians say. He called it the “Fever of Perinthus.” Others wonder whether this was flu, another illness, or a combination of illnesses.
“In 1173 and 1500, two other influenza outbreaks were described, though in scant detail. The name ‘influenza’ originated in the 15th century in Italy, from an epidemic attributed to the ‘influence of the stars,’” which, according to historical documents, “raged across Europe and perhaps in Asia and Africa,” a 2016 paper in the Journal of Preventive Medicine and Hygiene reported.
“Scholars and historians debate whether influenza was already present in the New World or whether it was carried by contaminated pigs transported on ships,” it added. “Some Aztec texts speak of a ’pestilential catarrh’ outbreak in 1450-1456 in an area now corresponding to Mexico, but these manuscripts are difficult to interpret correctly and this hypothesis seems controversial.”
What has all this got to do with COVID-19? There is an advantage to coming down with a virus that has been around for hundreds, if not a couple of thousand, years. Humans, ideally, will have built up more natural defenses to fight it.
Complicating matters: influenza and COVID-19 come from different virus families, and COVID-19 is brand new. “There are four other strains of the coronavirus, but the attack rate of this virus is relatively high as there is no immunity to it,” Adalja said.
To put that in perspective: In 2017–18, the worst flu season on record in the U.S. outside of a pandemic, approximately 80,000 Americans died. The four other coronavirus strains that already exist are responsible for around 25% of our common colds, Adalja added.
“But it doesn’t seem like there is cross-immunity with this coronavirus as there are with the other coronaviruses,” he added. In other words, the natural defense systems in our body that help us ward off flu are unlikely to apply here.
Luis Ostrosky, a member of the Infectious Diseases Society of America, said humans have a “herd immunity” to flu. “When there are enough people in the community who are immune it protects people who are not immune.” That is the case with flu, but not with COVID-19. Ostrosky said this is especially critical when no vaccines or therapeutic treatments for a virus.
“Both can be spread from person to person through droplets in the air from an infected person coughing, sneezing or talking,” Lisa Maragakis, senior director of infection prevention at Johns Hopkins Medicine in Baltimore, wrote. Based on the estimated distance viruses travel, scientists recommend “social distancing” of at least six feet in enclosed public spaces.
In the meantime, the virus continues to spread, likely helped by people who have mild symptoms or who are asymptomatic.
Worldwide, there were 126,135 COVID-19 cases and 4,630 deaths as of Wednesday evening; about 68,216 people have recovered, according to data published by the Johns Hopkins Whiting School of Engineering’s Center for Systems Science and Engineering. The U.S. has 1,311 confirmed cases, and has recorded at least 38 deaths.
 MarketWatch photo illustration/iStockphoto
MarketWatch photo illustration/iStockphoto While estimates of coronavirus fatality rates vary, they remain far higher than those for the flu. COVID-19 has a fatality rate of 3.4%, WHO director-general Tedros Adhanom Ghebreyesus said earlier this month. That’s more than previous estimates of between 1.4% and 2%, although some observers say his analysis was a blunt interpretation of incomplete data, and were probably skewed by a higher death rate in China.
COVID-19 rates may fall closer to those of the flu, assuming many more people are infected. JAMA recently released this paper analyzing data from the Chinese Center for Disease Control and Prevention on 72,314 COVID-19 cases in mainland China last month, the largest such sample of this kind. The sample’s overall case-fatality rate was 2.3%, in line with the earlier estimates.
‘As coronavirus spreads it threatens to put a much greater burden on health systems than flu does.’
Fatality rates also varied dramatically depending on the age of the individual. No deaths occurred in those 9 and younger, but cases in those aged 70 to 79 carried an 8% fatality rate, and those aged 80 years and older had a fatality rate of 14.8%. The rate was 49% among critical cases, and elevated among those with pre-existing conditions, to between 5.6% and 10.3%, depending on the condition.
Other differences between coronavirus and flu lie in what we don’t know. Adults with the flu, which has an average incubation period of two days, can infect others 24 hours before symptoms develop and 5 to 7 days after becoming sick. Novel coronavirus has a median incubation period of 5.1 days, longer than that other human coronaviruses (3 days) that cause the common cold.
The agency said the number of cases outside China has increased tenfold and the number of countries affected has tripled. “We expect to see the number of cases, the number of deaths and the number of affected countries climb even higher. WHO has been assessing this outbreak around the clock,” Tedros told reporters. “And we’re deeply concerned. Most by the alarming levels of spread and severity. And by the alarming levels of inaction.”
Coronavirus appears to be transmitted with ease to around 2.3 people by each person infected in the community, said Antigone Barton, editor of ScienceSpeaks, a medical website. Drug companies and the medical community, she said, are scrambling to come up with a vaccine before more people die, and health services are overwhelmed with sick people showing up at their doors.
The potential demand for hospital beds, ventilators, masks and medications, and the pressure all of this would put on staff worries her. “Because there’s no proven therapy or vaccine; as coronavirus spreads,” Barton said, “it threatens to put a much greater burden on health systems than flu does, and greater than most or many are prepared for.”
How COVID-19 is transmitted
div > iframe { width: 100% !important; min-width: 300px; max-width: 800px; } ]]>