On Thursday, U.S. Vice President Mike Pence toured a General Motors GM, -6.23% and Ventec ventilator production plant in Kokomo, Ind. and, in a decision that appeared to take into account the backlash to his last high-profile outing, he wore a mask.
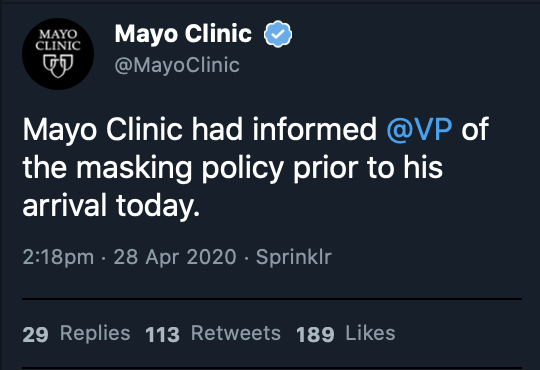
It was a turnaround from earlier in the week when he visited the Mayo Clinic without one and, according to the hospital, was told by hospital officials he should wear a mask. (The Rochester, Minn.-based hospital declined to comment beyond its official statement.)
But after that trip on Tuesday, Pence left a litany of serious questions behind at the Mayo Clinic, as doctors and medical ethicists were left aghast that the institution would put anybody’s wishes to eschew a mask, even a vice president’s, over safety protocol.
Why would a hospital, ranked No. 1 in the U.S., break its own policies and put its patients’ and medical staff’s health and even their lives at risk by allowing a visitor to walk around wards with no mask, no gown — and without maintaining the recommended six-feet distance?
“ ‘There’s a classic dilemma in health care: Celebrities and wealthy people get special treatment.’ ”
The Service Employees International Union roundly criticized the hospital’s decision to let Pence forgo a mask: “As the union that represents thousands of workers at Mayo, we are deeply disappointed that Mayo failed to enforce their own policy.”
The SEIU said that COVID-19, the disease caused by the novel coronavirus SARS-CoV-2, is preventable and treatable, “but only if we ensure working people are informed and protected.” The labor union represents around 2 million frontline health-care workers.
Many medical professionals were dismayed. “I would have said, ‘You’re not going in. You should be a good role model,’” said Art Caplan, director of medical ethics at the NYU Grossman School of Medicine. “You cannot deviate from procedure. It usually leads to bad outcomes.”
“The institution has an obligation first and foremost to make sure that all visitors are following their guidelines for safety for both patients and their staff,” he added. “That’s an absolute must. They have to enforce it, whether it’s the vice president or your 10-year-old child who’s visiting.”
Caplan lost his own mother, who was living in a nursing home, to COVID-19 on Monday. He told MarketWatch on Wednesday that he would, on this week, like to talk about how the nation’s health-care system needs to address inequity, and take action to help make things better.
Medical professionals say hospitals work tirelessly to develop and maintain positive relationships with state and federal officials who allocate crucial resources for medical institutions. That funding, they say, can impact everything from personal protective equipment to federal research grants.
The Mayo Clinic received $150 million in federal funds under the CARES Act as part of $1.2 billion disclosed by hospitals and health systems, according to Axios. The hospital was also awarded $142 million in funding in 2016 over five years by the National Institutes of Health.
Did funding influence the hospital’s decision? “The current administration is a bit of a slot machine,” said Augie Lindmark, resident physician at Yale Primary Care Residency Training Program at Yale University. “It’s unpredictable if, when, and how they’re going to spit cash into health systems.”
“I have no idea if Vice President Pence got push back from Mayo Clinic officials about not wearing a mask,” he added. “If the vice president shows up at your doorstep at a time when hospitals are getting massive infusions of federal funds, the red carpet is rolling out, with or without masks.”
Umbereen Sultana Nehal, a Boston, Mass.-based pediatrician, said a perceived balance of power may have influenced staff at the Mayo Clinic not to push the issue by asking Vice President Pence to wear a gown and a mask, or even maintain social distancing while speaking to patients.
“There may have been reticence to challenge authority of a VIP or a VP,” Nehal said. “There may have been a belief that Vice President Pence, as head of the national task force on coronavirus, had greater authority than hospital regulations. Hospitals are terrified of repercussions.”
“ ‘There may have been reticence to challenge authority of a VIP or a VP.’ ”
“Very little of what is being done right now is based on usual standards,” she added. “For instance, an N95 is meant to be a single use mask, not for use over a week or to be sterilized as has been happening. There are many shocking things going on right now.”
Nehal previously served as a chief medical officer and vice president of medical affairs for a federally qualified health center, or FQHC, where she had to ensure compliance with federal, state and city regulations, and sign off on clinical guidelines for safety and quality.
The Mayo Clinic later tweeted: “We are grateful that @VP and @GovTimWalz visited Mayo Clinic today to hear about our work fighting the #COVID19 pandemic. We look forward to continued collaboration to develop essential testing and treatment for our patients and communities.”
For his part, Pence told reporters after the visit, “As vice president of the United States I’m tested for the coronavirus on a regular basis, and everyone who is around me is tested for the coronavirus, and since I don’t have the coronavirus, I thought it’d be a good opportunity for me to be here.”
Pence gave another reason why he did not wear a mask, as recommended by the U.S. Centers for Disease Control and Prevention. He told reporters he wanted “to be able to speak to these researchers, these incredible health care personnel, and look them in the eye and say, ‘Thank you.’”
But Alison Bateman-House, assistant professor at the division of medical ethics at New York University, said Pence could have been infected with coronavirus shortly after his last COVID-19 test, adding that testing for the disease in the U.S. has not always been accurate.
She said the Mayo Clinic may not have wanted to deny the vice president access for fear of a public reprisal from President Donald Trump, particularly on Twitter TWTR, -2.92%. Although the White House advised the public to wear masks in public places, the president said he would not wear one.
“No hospital wants to be on the receiving end of a presidential tongue lashing,” she said. “To me that indicates a lack of moral courage. If you’re in the health-care profession, you have to do what’s best for public health and the population without worrying about Monday morning quarterbacking.”
The response to COVID-19 has become a political issue. President Trump and New York Gov. Andrew Cuomo have locked horns over when to reopen the economy. But Bateman-House said politics and patient safety don’t mix. “I don’t think this is a partisan issue at all,” she said.
Hospitals, she added, make hay from such high-profile visitors. “Any time you have a big name person come to your hospital, you use that news for fundraising and send it out to your donors.” This news, she said, is not worth sending. “Somebody seriously dropped the ball,” she added.
“ ‘Somebody seriously dropped the ball. I don’t think this is a partisan issue at all.’ ”
Bateman-House cited the case of Chicago Mayor Lori Lightfoot, a Democrat, who earlier this month defended her decision to get a haircut, while salons and barbershops were closed in her city. “I’m the public face of this city,” Lightfoot said. “I’m on national media and I’m out in the public eye.”
Caplan also said this issue goes beyond the Mayo Clinic. “There’s a classic dilemma in health care: Celebrities and wealthy people get special treatment,” he said. “If you’re going to put yourself forward as an honest broker of public-health information, it’s an embarrassing moment.”
He said the episode reveals deeper problems in the health-care system. “When the elite don’t follow public-health rules like everybody else and the powerful have special access, it’s a stark reminder of the inequity that underlies our health-care system due to money, celebrity status or connections.”
In mid-March, during a nationwide shortage of tests for COVID-19, the National Basketball Association said that at least eight teams had tested positive for the virus, leading the NBA to cancel the remainder of the games for the season.
Mayor Bill de Blasio tweeted: “We wish them a speedy recovery. But, with all due respect, an entire NBA team should NOT get tested for COVID-19 while there are critically ill patients waiting to be tested. Tests should not be for the wealthy, but for the sick.”
The numbers keep climbing. As of Friday, 6.2 million people had been tested in the U.S. for SARS-CoV-2. There were 1,102,703 confirmed cases, and 64,804 deaths in the U.S., of which 18,399 were in New York City. Worldwide, there were 3,127,126 confirmed cases and 213,792 deaths.
The wealthiest Americans have the money and the real estate and — in some cases their private yachts — to quarantine themselves and wait the pandemic out, while the lowest-paid Americans are showing up for work, and putting their health and lives on the line.
One-third of frontline workers are members of low-income households, and non-white households have been hard hit, Gov. Cuomo previously said. “We see the infection rate among African-Americans and brown Americans higher proportionally than other groups,” Cuomo said. “Why? Because they were out there exposing themselves.”
“I am calling on the federal government to provide hazard pay to these frontline workers and give them a 50% bonus because they are the true heroes in this crisis,” he said, adding, “Essential public workers are the ones on the front lines every day.”
“ One-third of frontline workers are from low-income households, and 40% of health-care staff are people of color. ”
His office cited recent data from the Center for Economic and Policy Research, which states that 41% of frontline workers are people of color. Of those, 45% of public transit workers and 40% of health-care workers are people of color, and this week he lauded them for showing up for work.
“What if they said, ‘You don’t pay me enough to put my life in danger? I’m not doing it.’ They showed up. They didn’t show up for a pay check. They didn’t show up because government asked them to show up,” he said. “They showed up out of their honor, out of their values, out of their dignity.”
The Mayo Clinic, meanwhile, touts its top spot in the nation, per the U.S. News & World Report. “Mayo Clinic has more No. 1 rankings than any other provider based on factors such as reputation, mortality index, patient safety, nurse staffing and Magnet status, patient services and technology.”
The clinic states on its website: “Mayo Clinic physicians, scientists, researchers, educators and allied health staff members work together in a team-based model to deliver the highest standards of care and transform scientific discoveries into critical advances for unmet patient needs.”
Medical ethicists and health-care workers say healthy relationships with powerful donors and lawmakers enables medical centers to secure the resources that help them become leaders in their field. However, those same ties can also lead to conflicts of interest and poor decisions, they add.
“A lot of clinicians have been treated like Cassandra where we get disregarded or sidelined, but our concerns about safety have turned out to be true,” Nehal, the Boston-based pediatrician, added. “There’s no joy in being right. I’d rather see good results that put patient safety first.”








Add Comment