Vaccines are a method of delayed antibody generation, and a vaccine for COVID-19 clearly would move us closer to resuming normal life.
Except a vaccine represents just one approach to dealing with COVID-19 and, most likely, is not the panacea that we all long for. Vaccine distribution will take time to reach all corners of the world. Not everyone can or will choose to vaccinate themselves and their loved ones, and, for those who do so, vaccines require one to two months to develop antibody protection. The elderly and immuno-compromised typically respond poorly to vaccines.
Even in the best-case scenario, vaccines would not provide a solution that is available tomorrow. A belt-and-suspenders approach — the development of safe, effective treatments along with the vaccine — provides multiple routes to ending the pandemic and our best shot at finding treatments that will work for everyone. We still need a therapeutic option for those who acquire COVID-19 — immediate treatment options that can reach the masses quickly.
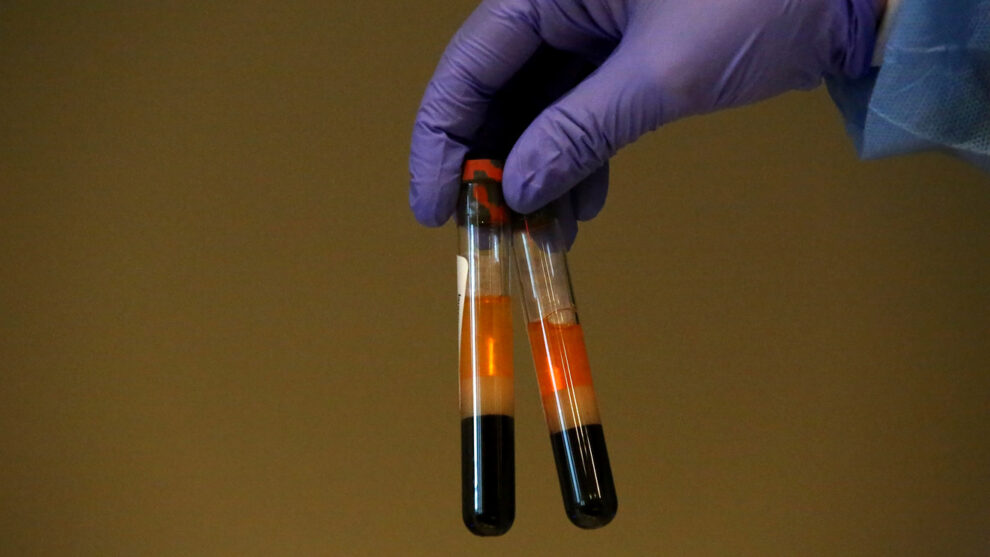
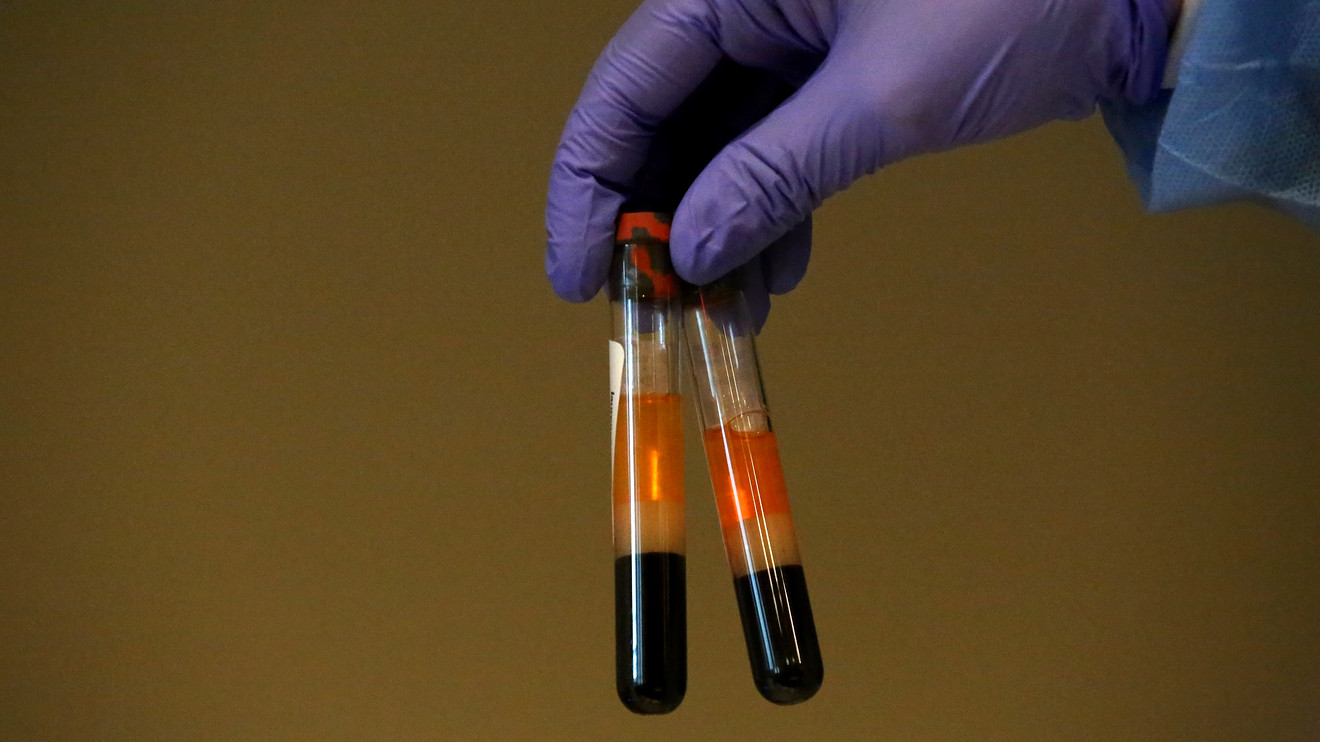
My colleagues at Johns Hopkins and I are exploring a potential new outpatient solution, using blood plasma from individuals who defeated COVID-19 and are fully recovered. Our two clinical trials are the first multi-center, double-blind, randomized studies of outpatient convalescent plasma, designed to meet the highest levels of scientific rigor and deliver the fastest results.
How does it work? The studies test how effective high-antibody-titer convalescent plasma is at treating COVID-19 in its early stages and in preventing those household members exposed to it from catching the disease. Half of the patients receive plasma with COVID-19 antibodies; the other half receive plasma with no antibodies. Our working theory is that a high-dose antibody treatment early on could help individuals recover faster, avoid hospitalization or avoid contracting COVID-19 entirely.
Filling a void in treatment and prevention
We are learning more every day about how COVID-19 works and ways to provide better care for patients who enter the hospital. But for life to get back to normal — even after a vaccine is approved — we will need multiple medical options at the ready to continue to fight the virus before someone gets sick enough to require hospitalization.
As we considered possible research pathways, we zeroed in on treating and preventing COVID-19 at its earliest stages and in outpatient settings, areas where no FDA-approved solutions exist yet. There is no outpatient therapy for COVID-19.
If these plasma trials prove successful in treating and preventing illness, the potential implications are vast. It could help ease anxieties around some of the most unnerving aspects of the virus, including long quarantine periods, which are highly disruptive, and the fear that otherwise healthy people will experience severe complications resulting in hospitalization.
Take, for example, how this treatment option could impact manufacturing sites. If one employee tests positive, every employee who was in close proximity would immediately receive a dose of plasma to avoid getting sick, and the infected employee would receive a dose to aid their recovery. It could bypass the need for numerous employees to quarantine for two weeks and keep operations running seamlessly.
A safe and effective early antibody treatment could reduce hospitalizations and deaths among the elderly and other high-risk groups. And it could provide much-needed reassurances for essential workers who must continue to serve on the front lines.
The U.S. Department of Defense, which is partially funding our research, is eager to protect the health of those serving in the military. Social distancing is nearly impossible in settings such as ships and aircraft carriers. Having an antibody treatment available to administer to everyone who is exposed in this type of setting could not only curb an outbreak, but also keep mission-critical endeavors on track. Importantly, a single dose of this immediate antibody immunity may result in protective antibody levels for three to six weeks.
What we know about blood plasma
Using convalescent plasma to treat COVID-19 makes sense for a variety of reasons.
First, there is history to consider. For more than 100 years, convalescent plasma therapy has proven safe and effective in treating and preventing other infectious outbreaks including childhood diphtheria, measles, Ebola and the 1918 influenza pandemic.
Second, it’s a naturally derived treatment. We don’t have to investigate the side effects of how an unknown pharmaceutical substance reacts inside the human body. Plasma is even very safe during pregnancy.
Third, the delivery method — blood transfusions — is already well-understood and highly regulated. It’s also an option that’s rapidly scalable. Complicated supply chains and manufacturing processes aren’t involved. The Red Cross and other organizations worldwide already have systems in place for people to donate plasma. Outpatient blood transfusions can take place in a diverse range of locations, from urgent-care centers to doctors’ offices to community health centers serving rural populations.
Of course, a blood infusion isn’t nearly as quick or convenient as a shot in the arm. It takes a few hours and the right blood type. But being choosy about options isn’t a luxury we are yet afforded.
Now, we need to understand if and how plasma can help fight off COVID-19. More than 100,000 hospitalized U.S. patients have already received successful convalescent plasma treatments. The Johns Hopkins clinical trials will examine plasma’s ability to stop progression of the virus early on. Its efficacy is being measured in several ways, including the ability to prevent hospitalization, spread to other household members and how long antibody protection lasts.
Ultimately, if we see positive outcomes, plasma could open new early treatment possibilities not only for COVID-19 but also other diseases.
Patients needed for clinical trials
Our research is not tethered to any corporate funding, and there is no intellectual-property ownership at stake. We may not be able to eradicate COVID-19 right now, but we are driven to find a way to make it less harmful and intrusive to our lives and livelihoods.
Johns Hopkins is conducting clinical trials with a variety of testing sites across the U.S. and in the Navajo nation to examine a diverse demographic. Clinical trials will run through the end of 2020. If all goes well, plasma treatments could be an option for the public in early 2021.
David Sullivan, M.D., is professor of molecular microbiology and immunology at the Johns Hopkins Bloomberg School of Public Health and a principal investigator for the Johns Hopkins Plasma Trials. To see if you qualify for the study, visit CovidPlasmaTrial.org or call 888-506-1199.
If you’re diagnosed with or exposed to COVID-19, or if you are a clinician working with patients who are, please follow health leaders’ guidance. Consider visiting CovidPlasmaTrial.org or calling the plasma trial’s call center at 1-888-506-1199 if you have a recent exposure or a new positive COVID test to learn more about how you can contribute to a solution.
More:To defeat COVID-19, ‘we need a unified national strategy,’ says public health expert Dr. Howard Koh