Two months into the epidemic, the coronavirus has not proven to be as deadly as the SARS virus. That, however, may also help explain why it’s spreading so quickly. It has an incubation period of up to two weeks, which enables the virus to spread through person-to-person contact.
The coronavirus, a pneumonia-causing illness that infects the respiratory tract, was responsible for at least 425 deaths and 20,438 infections as of Tuesday, according to China’s National Health Commission.
A 44-year-old man in the Philippines was the first person reported to die outside China from the virus, health officials in that country announced Sunday; he was from Wuhan, China, believed to be the epicenter of the outbreak. A man died from the virus in Hong Kong, according to media reports; he was 39 years of age and had also recently traveled from Wuhan.
Japan quarantined a cruise ship with 3,000 people on board after one passenger on the ship tested positive for the virus after leaving the vessel while it was in Hong Kong, the Associated Press reported.
SARS, or severe acute respiratory syndrome, infected 8,096 people worldwide with approximately 774 official SARS-related deaths; most of those infections occurred during a nine-month period from 2002 to 2003.
SARS had a fatality rate of 9.6% compared to coronavirus fatality rate of 2.1%, but that may change.
SARS had a fatality rate of 9.6% compared to the fatality rate of 2.1% so far for this new 2019-nCoV strain of coronavirus, according to MarketWatch calculations based on figures from WHO and China’s National Health Commission.
The fatality rate has remained steady for the last several weeks. However, that death toll could rise as the weeks progress. Whether the fatality rate will remain steady has yet to be determined.
Assuming an incubation period of up to 14 days, with an average of seven days before a person presents with symptoms of the virus, the current fatality rate may end up being higher than the eventual rate.
The current fatalities of 425 based on the total number of cases reported seven days ago (2,700) by Chinese health officials equates to a fatality rate of closer to 15.8%, based on MarketWatch calculations.
The opposite, however, may also be true.
If, on the other hand, the number of infections has been vastly under-counted, the 2.1% coronavirus fatality rate could fall, which would be good news for those who have contracted the illness. (The World Health Organization has declared a global health emergency.)
Maciej Boni, an associate professor of biology, at Pennsylvania State University, said the 2009 H1N1 flu pandemic initially overestimated the final fatality rate, while the SARS fatality rate rose as the virus spread.
Boni wrote on Jan. 30 on the online science magazine LiveScience, “During the 2009 influenza pandemic, the earliest reports listed 59 deaths from approximately 850 suspected cases, which suggested an extremely high case fatality of 7%. However, the initially reported information of 850 cases was a gross underestimate. This was simply due to a much larger number of mild cases that did not report to any health system and were not counted.”
“After several months — when pandemic data had been collected from many countries experiencing an epidemic wave — the 2009 influenza turned out to be much milder than was thought in the initial weeks. Its case fatality was lower than 0.1% and in line with other known human influenza viruses,” he added.
But even that fatality rate is lower than the SARS fatality rate. The difference in these two fatality rates gives more context as to why the coronavirus has spread so quickly. Medical experts say an effective flu-like virus can extend its reach by not killing its host too rapidly and/or making the host sick enough to pass it on before finally becoming bedridden.
“Every now and then a disease becomes so dangerous that it kills the host,” Matan Shelomi, an entomologist and assistant professor at National Taiwan University, wrote on Quora in 2017. But, ideally for the host at least, it must strike a balance.
“If the disease is able to spread to another host before the first host dies, then it is not too lethal to exist. Evolution cannot make it less lethal so long as it can still spread,” he added. “If a hypothetical disease eradicates its only host, both will indeed go extinct.”
‘The strain of the Black Death plague (Yersinia pestis) from the 14th Century was too virulent and is now extinct.’
That, he said, is why the Black Death, which ravaged much of Europe and Asia in the Middle Ages is now extinct. “The strain of the Black Death plague (Yersinia pestis) from the 14th Century was too virulent and is now extinct,” with only modern, less devastating strains in existence.
Animals are useful for viruses to jump humans. “The animal is the disease reservoir,” Shelomi wrote. “Even if all humans were vaccinated against such a disease, we’d need to vaccinate the animal reservoir too in order to eradicate the disease, which is impractical if not impossible.”
Sean Beckmann, assistant professor of Biology at Stetson University in Florida who is an expert in zoonotic infections, which jumped from animals to humans, told the life-science website BioSpace.com on Jan. 31 that there’s still a lot we don’t know about the new strain of coronavirus.
“It isn’t something that looks like it can hang out on surfaces or in the air for a long time and still be infectious,” he said. “It looks like it requires pretty close contact, which is why outside this epicenter in China we’re not seeing a lot of human-to-human transmissions.”
“This does not look like a virus that is able to stay alive in the air or on surfaces for a very long time. Which is good,” he added.
Other far more deadly viruses have taken more than half a century to become a global epidemic. For instance, it’s widely understood that HIV originated in Kinshasa in the Democratic Republic of Congo around 1920 when the virus crossed over from chimpanzees to humans.
“Up until the 1980s, we do not know how many people were infected with HIV or developed AIDS. HIV was unknown and transmission was not accompanied by noticeable signs or symptoms,” according to Avert.org, a global information and education resource on the disease.
Recommended: This is how the illness has spread across the world so rapidly
HIV/AIDS has an incubation period of 40 to 60 days, although that can vary wildly. “The current epidemic started in the mid to late 1970s,” Avert said. “By 1980, HIV may have already spread to five continents. In this period, between 100,000 and 300,000 people could have already been infected.”
But the virus took hold in the years following the sexual revolution, with the first reported cases in the U.S. among gay men in 1981 and intravenous drug users. Untreated, it has a fatality rate of almost 100%. To date, 75 million people have contracted HIV with an estimated 32 million deaths.
Like HIV, the coronavirus has created its own brand of fear and loathing. Rumors about whether it began in a food market in Wuhan have led to allegations of racism against Chinese people in Canada, the U.K., Malaysia and South Korea, and elsewhere, and xenophobic comments online.
Chinese President Xi Jinping told the World Health Organization head Tedros Adhanom Ghebreyesus last week, “Chinese people are currently engaged in a serious struggle against an epidemic of a new type of coronavirus infection. The epidemic is a demon, and we cannot let this demon hide.”
Other deadly viruses have taken more than half a century to become a global epidemic.
However, reports that more than half-a-dozen doctors first discussed the threat of a potential coronavirus outbreak in early December only to be silenced by the local Communist Party has led critics to speculate that more could have been done after the first diagnosis.
Yaxue Cao, founder and editor of the political pressure group ChinaChange.org, said a Wuhan doctor said in a WeChat group in late December that there were “7 cases of SARS connected to the seafood market.” He was then scolded by the party disciplinary office, and forced to retract that, Cao said.
“From the same report, we learned that Wuhan health authorities were having overnight meetings about the new ‘SARS’ at end of December,” Cao posted on Twitter Jan. 27. “Earlier today the Wuhan mayor said he was not ‘authorized’ to publicize the epidemic until Jan. 20.”
Wuhan mayor Zhou Xianwang said 5 million people had left the city before travel restrictions were imposed ahead of the Chinese New Year. Ma Xiaowei, the director of China’s National Health Commission, said that the virus had an incubation period of up to 14 days.
China has taken major steps to help prevent the spread of the virus. Officials in Wuhan, a city of 11 million residents that is widely regarded as the epicenter of the illness, closed the area’s outgoing airport and railway stations and suspended all public transport.
Chinese officials have expanded that travel ban to 16 surrounding cities with a combined population of more than 50 million people, including Huanggang, a neighboring city to Wuhan with 7.5 million people, effectively putting those cities on lock down.
The Wall Street Journal reported that some families in China have voiced concern and frustration that their relatives’ cause of death was marked as “severe pneumonia” or “viral pneumonia” on their death certificates.
Beckman also told Biospace.com that efforts to contain coronavirus happen in three stages: “You get containment and trying to reduce the spread as much as possible. You get the development of symptomatic treatment, things like antivirals. And the third one, and the more long-term process, is vaccine development. And that’s because vaccine development takes quite a bit of time.”
The Centers for Disease Control and Prevention last week confirmed the first case of person-to-person spread of coronavirus in Illinois. There were 11 confirmed cases of coronavirus in the U.S. as of Monday, according to the Centers for Disease Control and Prevention, and state health officials.
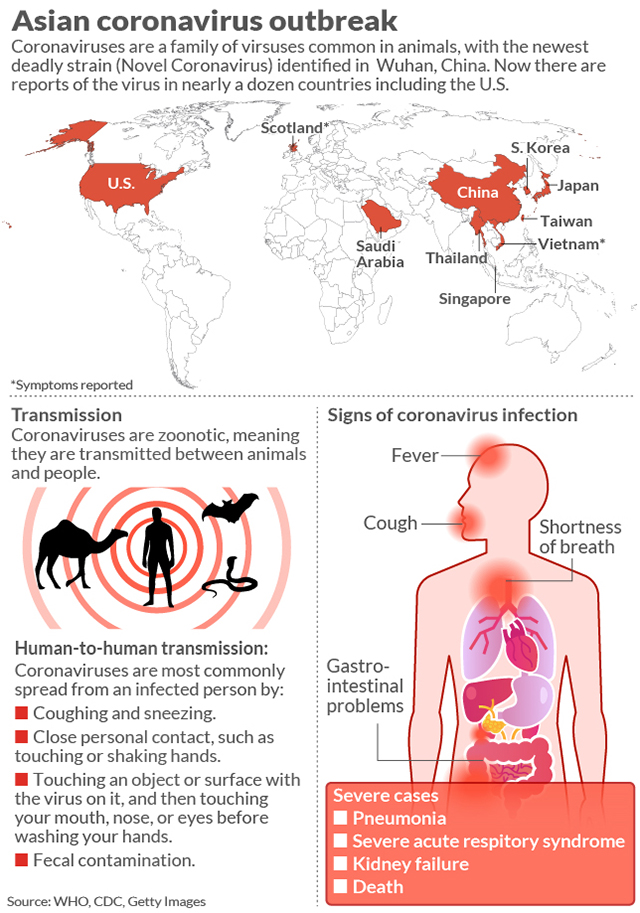
According to figures provided by the CDC, there are confirmed cases in two dozen countries or territories, including Germany, Japan, Vietnam, and the U.S., the U.K. and Russia. On Sunday, New York City health officials said two more patients there were being tested for coronavirus, bringing the total of suspected cases in that state to three.
So will the latest coronavirus outbreak be more similar to the 2002-2003 SARS outbreak or the 2009 H1N1 influence pandemic? Boni wrote on LiveScience: “I am a professor of biology who studies the evolution and epidemiology of infectious disease, and in my view, in late January 2020, we do not yet have enough solid evidence to answer this question.”
This story was originally published on Jan. 30 and has been updated.



